A Chasm of Misunderstanding
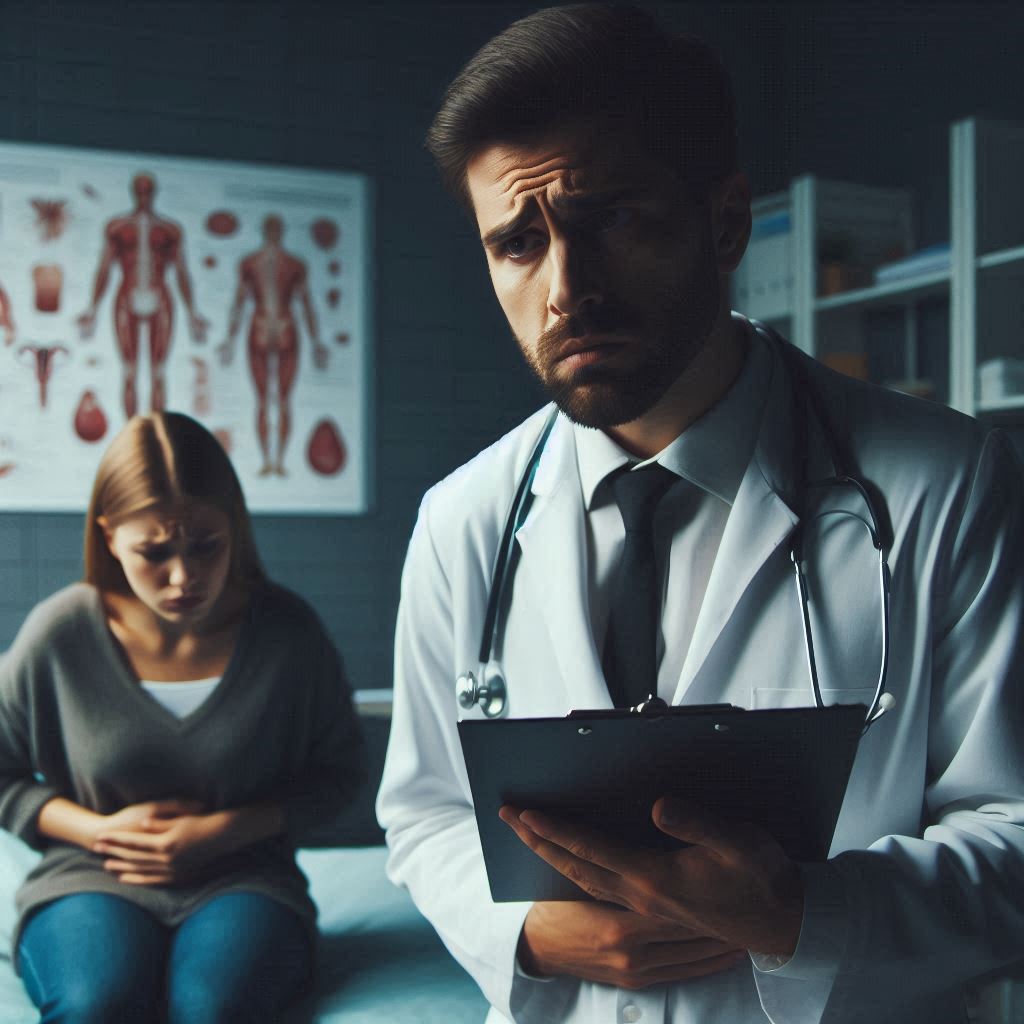
A recent study conducted by researchers at the University of Cambridge sheds light on a troubling trend in healthcare—the misdiagnosis of chronic autoimmune diseases as psychosomatic or psychiatric disorders. This phenomenon, often characterized by a ‘**chasm of misunderstanding** and miscommunication’ between patients and clinicians, has significant implications for patient health and overall well-being.
Misdiagnosed autoimmune conditions, such as **lupus** and **vasculitis**, can lead to unchecked physical deterioration and psychological distress. The study, involving over **3,000 participants**, revealed that such misdiagnoses could trigger a broad spectrum of negative impacts on patients’ lives, cultural perceptions of illness, and even their mental health. Notably, patients often described feeling dismissed, with one participant recalling a doctor stating, “**You’re making yourself feel pain.**” Such statements can linger hauntingly, leading to increased **anxiety** and **depression**.
Understanding Autoimmune Diseases
Autoimmune rheumatic diseases, including **rheumatoid arthritis**, **lupus**, and **vasculitis**, pose a diagnostic challenge due to their diverse and often invisible symptoms. Patients frequently report issues like **extreme fatigue** and **depression**, which can be misleading and lead to misinterpretations by healthcare providers. According to Dr. Melanie Sloan, who led the Cambridge study, these conditions affect the **immune system** and can have long-lasting consequences on multiple bodily systems.
The complexity of these diseases often results in a diagnostic lag. Clinicians may struggle to identify them due to their wide variance in presentation; symptoms are often **non-specific**, leading to misdiagnoses as mental health conditions. In the study, a substantial proportion of patients indicated feeling their **self-worth** diminished as a result of being misdiagnosed. Over **80%** reported adverse effects on their overall mental wellness, with **72%** indicating ongoing distress related to their misdiagnosis years later.
The Psychological Toll of Misdiagnosis
The emotional fallout from misdiagnosis can be just as alarming as the physical ramifications. For instance, many individuals stated they began to **self-blame** for their illnesses post-misdiagnosis. This self-perception can spiral into severe emotional distress, leading patients to avoid medical help altogether due to a lack of trust in healthcare professionals. One patient articulated this sentiment starkly: “**I don’t deserve help because this is a disease I’ve brought on myself.**” In such cases, mental health challenges become compounded over time, straining the patient’s relationship with medical providers and deepening their isolation.
The study unearthed several disturbing accounts, including one patient whose suicidal tendencies intensified following dismissive comments from medical professionals. They described how feeling **gaslit** by a clinician compounded their existing distress. The fallout from such interactions not only diminishes a patient’s trust but also complicates the recovery process when a proper diagnosis is finally reached.
Rebuilding Trust: A Path Forward
The research highlights a vital need for clinicians to cultivate a **holistic understanding** of autoimmune diseases. Doctors must recognize the psychological consequences that misdiagnosis can inflict on patients. Insights shared in the study support the idea that open communication can help mend the patient-physician relationship.
A noteworthy example from the study featured a patient who felt previously **gaslit** by their clinician. Upon addressing this with the doctor, the clinician showed genuine remorse, demonstrating how a simple acknowledgment can radically transform a patient’s experience. Patients reported that transparency and acknowledgement of past misdiagnoses led to healing, both physically and emotionally. Such responsiveness from healthcare providers can foster patient trust and influence future healthcare behaviors.
Recommendations for Change in Medical Practice
The authors of the study propose various strategies aimed at fostering patient trust and understanding among healthcare providers. These include:
1. **Open Dialogue**: Clinicians should engage in direct conversations about prior misdiagnoses to acknowledge their impact on patients’ mental health.
2. **Empathetic Engagement**: Empathy can help healthcare providers form a connection with patients and better understand their experiences.
3. **Increased Access to Psychological Care**: Health services should provide greater access to psychologists and supportive therapies, particularly for patients who have experienced misdiagnosis.
4. **Training and Education**: Educating clinicians about autoimmune diseases’ systemic and varied presentations can significantly reduce the risk of misdiagnosis.
As co-author Mike Bosley emphasized, a critical paradigm shift is needed in medical practice. “All clinicians must appreciate that autoimmune conditions can present in unusual ways and that listening carefully to patients is key to avoiding long-lasting harm.**”
Professor Felix Naughton, an expert in the field, echoed these sentiments, noting that with increased clinical awareness and more training, the risk of misdiagnosis can be reduced. This proactive approach could significantly improve outcomes for patients currently suffering in silence.
This study serves as a crucial reminder of the broader societal implications of misdiagnosis and the need for a more compassionate healthcare system. Educating healthcare professionals could bridge the current gap in understanding and promote a more supportive environment for those living with chronic diseases.
To learn about the disclaimer of liability for the content of this website, click here